Bursitis Of The Feet Medical Procedures
Bursae (two or more bursa) are small, fluid-filled sacs that cushion the bones, tendons and muscles surrounding your joints. They contain a lubricating fluid that reduces friction, allowing tissues in the body to glide past each other smoothly. Imagine the bursa as a protective layer that helps keep a tendon or muscle from fraying or getting aggravated as it eases over a bone or around a corner. Bursitis is a condition that occurs when a bursa becomes inflamed: irritated, red and filled with more fluid than normal.
Causes
Retrocalcaneal bursitis is generally caused by local trauma from poorly designed shoes. Patients complain of posterolateral heel pain and may have a posterior heel prominence (?pump bump?), as well as local swelling and tenderness over the Achilles tendon. Pain is increased by squeezing the bursa from side to side and anterior to the Achilles. A heel lift and open-back shoes help alleviate pressure.
Symptoms
Symptoms of bursitis usually occur after rest and relaxation. Upon activity there is usually more intense pain in the area of the bursa. The common areas to have a bursitis in the foot are in the bottom of the heel, behind the heel near the attachment of the Achilles Tendon as well as along the side of a bunion. A bursa may also form in multiple areas especially along the metatarsal heads, or "ball" of your foot. You may actually feel the sac like fluid when rubbing the area of pain.
Diagnosis
In addition to a complete medical history and physical examination, diagnostic procedures for bursitis may include the following. X-ray. A diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film. Magnetic resonance imaging (MRI). A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. Ultrasound. A diagnostic technique that uses high-frequency sound waves to create an image of the internal organs. Aspiration. A procedure that involves removal of fluid from the swollen bursa to exclude infection or gout as causes of bursitis. Blood tests. Lab tests that are done to confirm or eliminate other conditions.
Non Surgical Treatment
The following exercises are commonly prescribed to patients with retrocalcaneal bursitis. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 2, 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Move your foot and ankle up and down as far as you can go without pain and provided you feel no more than a mild to moderate stretch. Repeat 10, 20 times provided there is no increase in symptoms. Move your foot and ankle in and out as far as you can go without pain and provided you feel no more than a mild to moderate stretch. Repeat 10, 20 times provided there is no increase in symptoms. Move your foot and ankle in a circle as large as you can go without pain and provided you feel no more than a mild to moderate stretch. Repeat 10, 20 times in both clockwise and anticlockwise directions provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head as far as you can go without pain and provided you feel no more than a mild to moderate stretch in the back of your calf, Achilles tendon or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free.
Surgical Treatment
Surgery. Though rare, particularly challenging cases of retrocalcaneal bursitis might warrant a bursectomy, in which the troublesome bursa is removed from the back of the ankle. Surgery can be effective, but operating on this boney area can cause complications, such as trouble with skin healing at the incision site. In addition to removing the bursa, a doctor may use the surgery to treat another condition associated with the retrocalcaneal bursitis. For example, a surgeon may remove a sliver of bone from the back of the heel to alter foot mechanics and reduce future friction. Any bone spurs located where the Achilles attaches to the heel may also be removed. Regardless of the conservative treatment that is provided, it is important to wait until all pain and swelling around the back of the heel is gone before resuming activities. This may take several weeks. Once symptoms are gone, a patient may make a gradual return to his or her activity level before their bursitis symptoms began. Returning to activities that cause friction or stress on the bursa before it is healed will likely cause bursitis symptoms to flare up again.
New Hammer Toe Surgery
 Overview
Overview
Uneven muscle tension results in the distortion of one or several of the small toes. (hammertoe) Pressure points develop at the raised middle joint as well as at the tip of the toe and underneath the metatarsal head. In the beginning, when the misalignment can still be corrected, it often suffices to lengthen the tendon and to cut a notch into the capsule. In a contracted misalignment, part of the middle joint is removed to form a replacement joint. Modern surgical techniques preserve the metatarsophalangeal joint (Weil or Helal osteotomies).
Causes
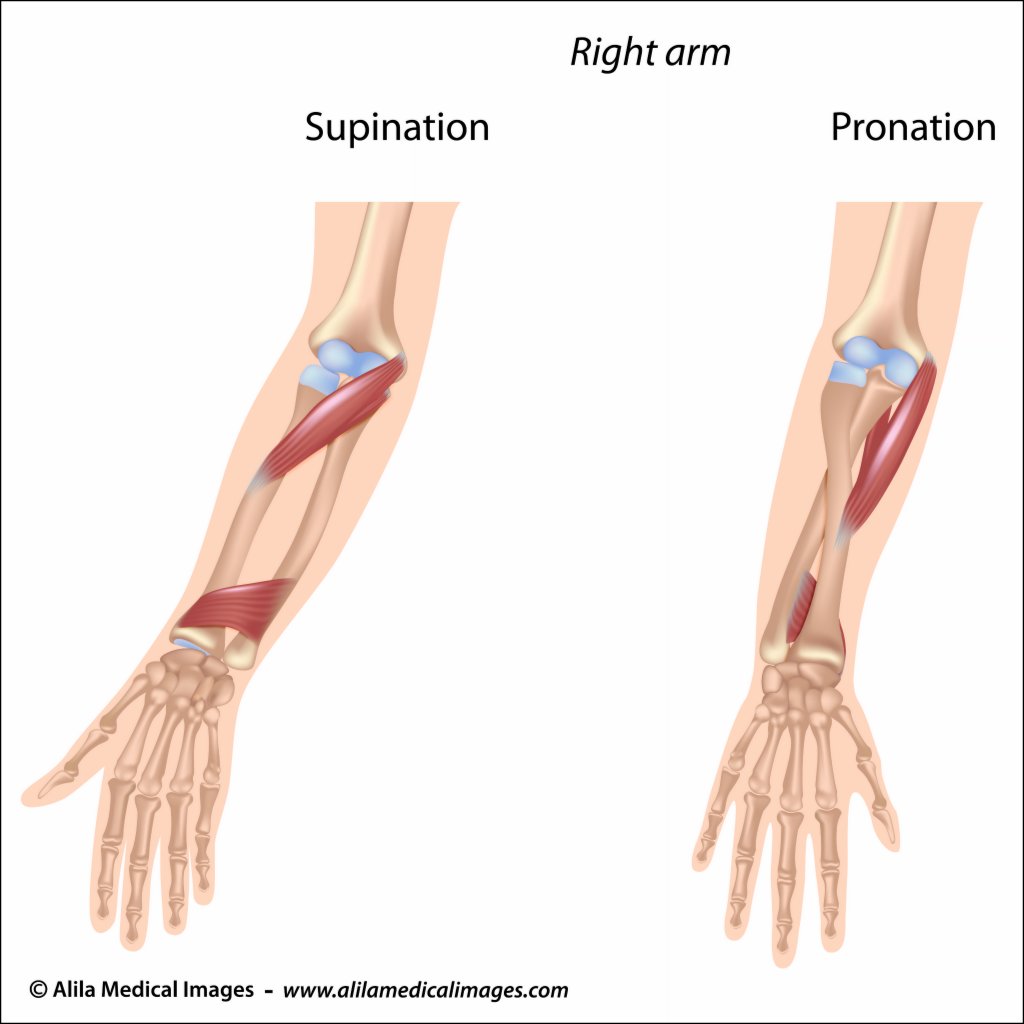
If a foot is flat (pes planus, pronated), the flexor muscles on the bottom of the foot can overpower the others because a flatfoot is longer than a foot with a normal arch. When the foot flattens and lengthens, greater than normal tension is exerted on the flexor muscles in the toes. The toes are not strong enough to resist this tension and they may be overpowered, resulting in a contracture of the toe, or a bending down of the toe at the first toe joint (the proximal interphalangeal joint) which results in a hammertoe. If a foot has a high arch (pes cavus, supinated), the extensor muscles on the top of the foot can overpower the muscles on the bottom of the foot because the high arch weakens the flexor muscles. This allows the extensor muscles to exert greater than normal tension on the toes. The toes are not strong enough to resist this tension and they may be overpowered, resulting in a contracture of the toe, or a bending down of the toe at the first toe joint (the proximal interphalangeal joint) which results in a hammertoe.
 Symptoms
Symptoms
Symptoms include sharp pain in the middle of the toe and difficulty straightening the toe. People with hammertoe may also develop blisters, which are fluid-filled pockets of skin, because the bent toe is likely to rub against the inside of a shoe. This increased friction may also lead to calluses, which are areas of thickened skin, and corns, which are hard lumps that may form on or between toes. Symptoms may be minor at first, but they can worsen over time.
Diagnosis
Although hammertoes are readily apparent, to arrive at a diagnosis the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. During the physical examination, the doctor may attempt to reproduce your symptoms by manipulating your foot and will study the contractures of the toes. In addition, the foot and ankle surgeon may take x-rays to determine the degree of the deformities and assess any changes that may have occurred.
Non Surgical Treatment
Mild hammer toe in children can be treated by manipulating and splinting the affected toe. The following changes in footwear may help relieve symptoms. Wear the right size shoes or shoes with wide toe boxes for comfort, and to avoid Hammer toe making hammer toe worse. Avoid high heels as much as possible. Wear soft insoles to relieve pressure on the toe. Protect the joint that is sticking out with corn pads or felt pads. A foot doctor can make foot devices called hammer toe regulators or straighteners for you, or you can buy them at the store. Exercises may be helpful. You can try gentle stretching exercises if the toe is not already in a fixed position. PIcking up a towel with your toes can help stretch and straighten the small muscles in the foot.
Surgical Treatment
Hammertoe surgery is performed when conservative measures have been exhausted and pain or deformity still persists. The surgery is performed on an outpatient basis. It typically required about one hour of time. An incision is placed over the inter-phalangeal joint. Once the bone is exposed, the end portion of the bone is removed. Your surgeon may then use pins or other fixation devices to assist in straightening the toe. These devices may be removed at a later date if necessary. Recovery for hammertoe surgery is approximately 10 to 14 days. You are able to walk immediately following the surgery in a surgical shoe. Swelling may be present but is managed as needed. Physical therapy is used to help reduce swelling in the toe or toes after surgery. Most of these toe surgeries can be performed in the office or the outpatient surgery under local anesthesia.
What Could Cause Painful Bunions?
Overview
 The common bunion is a localized area of enlargement of the inner portion of the joint at the base of the big toe. The enlargement actually represents additional bone formation, often in combination with a misalignment of the big toe. The misalignment causes the big toe to move outward (medically termed hallux valgus deformity). The normal position of the big toe (straight forward) becomes outward directed toward the smaller toes. The enlarged joint at the base of the big toe (the first metatarsophalangeal joint, or MTP joint) can become inflamed with redness, tenderness, and pain. A small fluid-filled sac (bursa) adjacent to the joint can also become inflamed (bursitis), leading to additional swelling, redness, and pain. A less common bunion is located at the joint at the base of the smallest (fifth) toe. This bunion is sometimes referred to as a tailor's bunion.
The common bunion is a localized area of enlargement of the inner portion of the joint at the base of the big toe. The enlargement actually represents additional bone formation, often in combination with a misalignment of the big toe. The misalignment causes the big toe to move outward (medically termed hallux valgus deformity). The normal position of the big toe (straight forward) becomes outward directed toward the smaller toes. The enlarged joint at the base of the big toe (the first metatarsophalangeal joint, or MTP joint) can become inflamed with redness, tenderness, and pain. A small fluid-filled sac (bursa) adjacent to the joint can also become inflamed (bursitis), leading to additional swelling, redness, and pain. A less common bunion is located at the joint at the base of the smallest (fifth) toe. This bunion is sometimes referred to as a tailor's bunion.
Causes
The most important causative factor is poor fitting footwear. This accounts for an higher incidence among women than men. Family history of bunions. Abnormal foot function, excessive pronation. Poor foot mechanics, such as excessive pronation (rolling inwards of the foot), causes a medial force which exerts pressure and can lead to the formation of bunions. Rheumatoid or osteoarthritis. Genetic and neuromuscular diseases, which can result in a muscular imbalance such as Down's syndrome. If one leg is longer then the other, the longer leg is more inclined to develop a bunion. If the ligaments in the feet are very weak. In some cases, bunions can occur due to trauma or injury to the feet.
Symptoms
The most common symptoms associated with this condition are pain on the side of the foot just behind the great toe. A red painful bump is usually present. Pain is usually brought on with walking or sports. Shoes don't cause bunions but will typically aggravate them. Stiff leather shoes or shoes with a tapered toe box are the prime offenders. This is why bunion pain is most common in women whose shoes have a pointed toe box. The bunion site will often be slightly swollen and red from the constant rubbing and irritation of a shoe. Occasionally, corns can develop between the 1st and 2nd toe from the pressure the toes rubbing against each other.
Diagnosis
Bunions are readily apparent, you can see the prominence at the base of the big toe or side of the foot. However, to fully evaluate your condition, the Podiatrist may arrange for x-rays to be taken to determine the degree of the deformity and assess the changes that have occurred. Because bunions are progressive, they don't go away, and will usually get worse over time. But not all cases are alike, some bunions progress more rapidly than others. There is no clear-cut way to predict how fast a bunion will get worse. The severity of the bunion and the symptoms you have will help determine what treatment is recommended for you.
Non Surgical Treatment
Nonsurgical treatments that may relieve the pain and pressure of a bunion include changing shoes. Wear roomy, comfortable shoes that provide plenty of space for your toes. Padding and taping or splinting. Your doctor can help you tape and pad your foot in a normal position. This can reduce stress on the bunion and alleviate your pain. Medications. Acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve) can help you control the pain of a bunion. Cortisone injections also can be helpful. Shoe inserts. Padded shoe inserts can help distribute pressure evenly when you move your feet, reducing your symptoms and preventing your bunion from getting worse. Over-the-counter arch supports can provide relief for some people, although others may require prescription orthotic devices. Applying ice. Icing your bunion after you've been on your feet too long can help relieve soreness and inflammation. 
Surgical Treatment
Bunions can cause pain and difficulty wearing certain shoes. When simple treatments don't relieve your symptoms, surgery may be considered for treatment of the bunion. What are the signs that surgery may be the right treatment for your bunion? In general, surgery is recommended only when pain from the bunion prevents a patient from wearing normal shoes. There is a common misconception that surgical treatments for a bunion are better and quicker than non-surgical treatments. Unfortunately, patients who rush into surgery may have unrealistic expectations, and may be unsatisfied with surgery.
Prevention
There are some steps that may help prevent, or at least slow, the progression of bunions. Avoid shoes with a narrow toe box. If your foot flattens excessively, make sure you wear supportive shoes, and if necessary, get custom orthotics from your podiatrist. See your podiatrist at the first signs or symptoms of a bunion deformity, as early treatment may stop or slow its progression.
Do You Know The Key Reasons Behind Over-Pronation
Pronation is the natural way that our feet absorb shock: when our feet strike the ground the arches flex down and in to disperse the impact. Everyone pronates! Contrary to popular misconception it is healthy and normal. The problem begins when one or both of our feet pronate too much. When the arches flex too far inward or stay collapsed for too long pronation is considered excessive. We call this overpronation. The amount of overpronation can vary from mild to severe. In severe overpronation the feet and ankles can rotate too far inward just during standing.

Causes
Generally fallen arches are a condition inherited from one or both parents. In addition, age, obesity, and pregnancy cause our arches to collapse. Being in a job that requires long hours of standing and/or walking (e.g. teaching, retail, hospitality, building etc) contributes to this condition, especially when standing on hard surfaces like concrete floors. Last, but not least unsupportive footwear makes our feet roll in more than they should.
Symptoms
Overpronation can lead to injuries and pain in the foot, ankle, knee, or hip. Overpronation puts extra stress on all the bones in the feet. The repeated stress on the knees, shins, thighs, and pelvis puts additional stress on the muscles, tendons, and ligaments of the lower leg. This can put the knee, hip, and back out of alignment, and it can become very painful.
Diagnosis
People who overpronate have flat feet or collapsed arches. You can tell whether you overpronate by wetting your feet and standing on a dry, flat surface. If your footprint looks complete, you probably overpronate. Another way to determine whether you have this condition is to simply look at your feet when you stand. If there is no arch on the innermost part of your sole, and it touches the floor, you likely overpronate. The only way to truly know for sure, however, is to be properly diagnosed by a foot and ankle specialist.
Non Surgical Treatment
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improper fitting footwear can lead to additional problems of the foot.
Prevention
Duck stance: Stand with your heels together and feet turned out. Tighten the buttock muscles, slightly tilt your pelvis forwards and try to rotate your legs outwards. You should feel your arches rising while you do this exercise.
Calf stretch:Stand facing a wall and place hands on it for support. Lean forwards until stretch is felt in the calves. Hold for 30 seconds. Bend at knees and hold for a further 30 seconds. Repeat 5 times.
Golf ball:While drawing your toes upwards towards your shins, roll a golf ball under the foot between 30 and 60 seconds. If you find a painful point, keep rolling the ball on that spot for 10 seconds.
Big toe push: Stand with your ankles in a neutral position (without rolling the foot inwards). Push down with your big toe but do not let the ankle roll inwards or the arch collapse. Hold for 5 seconds. Repeat 10 times. Build up to longer times and fewer repetitions.
Ankle strengthener: Place a ball between your foot and a wall. Sitting down and keeping your toes pointed upwards, press the outside of the foot against the ball, as though pushing it into the wall. Hold for 5 seconds and repeat 10 times.
Arch strengthener: Stand on one foot on the floor. The movements needed to remain balanced will strengthen the arch. When you are able to balance for 30 seconds, start doing this exercise using a wobble board.
Physical Therapy For Calcaneal Apophysitis
Sever's disease or Calcaneal apophysitis is a condition that affects children between the ages of 10 and 13 years. It is characterized by pain in one or both heels with walking. During this phase of life, growth of the bone is taking place at a faster rate than the tendons. Hence there is a relative shortening of the heel-cord compared to the leg bones. As a result, the tension the heel-cord applies to the heel bone at its insertion is very great. Moreover, the heel cord is attached to a portion of the calcaneus (heel bone) that is still immature, consisting of a mixture of bone and growing cartilage, called the calcaneal apophysis, which is prone to injury. Compounding to this is the fact that all these changes are happening in a very active child, prone to overuse. The end result is therefore an overuse syndrome of injury and inflammation at the heel where the heel cord (Achilles Tendonitis) inserts into the heel bone (Calcaneal apophysitis).
Causes
Sever?s disease is often associated with a growth spurt, when the bones grow but the muscles do not. Therefore the muscles effectively become tighter which results in increased stress at the heel. It may also be related to unusual biomechanics, for instance poor foot posture, muscle tightness or muscle weakness. Overtraining or incorrect training can also play a part. Usually, the cause is a combination of factors.
Symptoms
Pain is usually felt at the back of the heel and around the sides of the heel. If you squeeze the back of the heel from both sides simultaneously and pain is experienced Sever?s disease is more than likely present.
Diagnosis
A doctor or other health professional such as a physiotherapist can diagnose Sever?s disease by asking the young person to describe their symptoms and by conducting a physical examination. In some instances, an x-ray may be necessary to rule out other causes of heel pain, such as heel fractures. Sever?s disease does not show on an x-ray because the damage is in the cartilage.
Non Surgical Treatment
If the problem is bad enough, it is important to totally rest the symptomatic foot. Take a break from sport activity until the pain has significant improvement. Severe cases will need to be treated with a cast boot. Anti-inflammatory treatments include Icing, Over-the-counter anti-inflammatory medicine as recommended by your pediatrician or podiatrist. Shock absorption and support. Don't go barefoot at home, wear some type of good sandal or shoe. A significant and/or chronic case should be treated with prescription orthotics. This addresses mechanical problems that cause this problem, Using an over-the-counter heel cushion inside of the shoe, Athletic foot taping, Stretching. Runners stretch to stretch out the calf muscle. A night splint will also help. Severe or chronic cases respond best to prescription orthotics with specific modifications for this problem. May require a night splint. Daytime braces that may also help.
Prevention
To reduce the risk of heel pain or sore heels from Sever?s Disease. Only wear properly fitting shoes. A lace up shoe with a firm heel counter. Stretch calf and foot before exercising or playing sports. Properly taping the foot provides excellent protection and immediate pain relief. Wear shoe inserts or an over-the-counter orthotic. If the problem persists, consult your foot doctor.
Posterior Tibial Tendon Dysfunction Surgery Success
Overview
Adult flatfoot refers to a deformity that develops after skeletal maturity is reached. Adult flatfoot should be differentiated from constitutional flatfoot, which is a common congenital non-pathologic foot morphology. There are numerous causes of acquired adult flatfoot, including fracture or dislocation, tendon laceration, tarsal coalition, arthritis, neuroarthropathy, neurologic weakness, and iatrogenic causes. 
Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot deformity. There is often no specific event that starts the problem, such as a sudden tendon injury. More commonly, the tendon becomes injured from cumulative wear and tear. Posterior tibial tendon dysfunction occurs more commonly in patients who already have a flat foot for other reasons. As the arch flattens, more stress is placed on the posterior tibial tendon and also on the ligaments on the inside of the foot and ankle. The result is a progressive disorder.
Symptoms
The first stage represents inflammation and symptoms originating from an irritated posterior tibial tendon, which is still functional. Stage two is characterized by a change in the alignment of the foot noted on observation while standing (see above photos). The deformity is supple meaning the foot is freely movable and a ?normal? position can be restored by the examiner. Stage two is also associated with the inability to perform a single-leg heel rise. The third stage is dysfunction of the posterior tibial tendon is a flatfoot deformity that becomes stiff because of arthritis. Prolonged deformity causes irritation to the involved joints resulting in arthritis. The fourth phase is a flatfoot deformity either supple (stage two) or stiff (stage 3) with involvement of the ankle joint. This occurs when the deltoid ligament, the major supporting structure on the inside of the ankle, fails to provide support. The ankle becomes unstable and will demonstrate a tilted appearance on X-ray. Failure of the deltoid ligament results from an inward displacement of the weight bearing forces. When prolonged, this change can lead to ankle arthritis. The vast majority of patients with acquired adult flatfoot deformity are stage 2 by the time they seek treatment from a physician.
Diagnosis
Observation by a skilled foot clinician and a hands-on evaluation of the foot and ankle is the most accurate diagnostic technique. Your Dallas foot doctor may have you do a walking examination (the most reliable way to check for the deformity). During walking, the affected foot appears more pronated and deformed. Your podiatrist may do muscle testing to look for strength deficiencies. During a single foot raise test, the foot doctor will ask you to rise up on the tip of your toes while keeping your unaffected foot off the ground. If your posterior tendon has been attenuated or ruptured, you will be unable to lift your heel off the floor. In less severe cases, it is possible to rise onto your toes, but your heel will not invert normally. X-rays are not always helpful as a diagnostic tool for Adult Flatfoot because both feet will generally demonstrate a deformity. MRI (magnetic resonance imaging) may show tendon injury and inflammation, but can?t always be relied on for a complete diagnosis. In most cases, a MRI is not necessary to diagnose a posterior tibial tendon injury. An ultrasound may also be used to confirm the deformity, but is usually not required for an initial diagnosis.
Non surgical Treatment
Get treated early. There is no recommended home treatment. While in stage one of the deformity, rest, a cast, and anti-inflammatory therapy can help you find relief. This treatment is followed by creating custom-molded foot orthoses and orthopedic footwear. These customized items are critical in maintaining the stability of the foot and ankle. Once the tendon has stretched and deformity is visible, the chances of success for non-surgical treatment are significantly lower. In a small percentage of patients, total immobilization may arrest the progression of the deformity. A long-term brace known as an ankle foot orthosis is required to keep the deformity from progressing. The Richie Brace, a type of ankle foot orthosis, shows significant success as a treatment for stage two posterior tibial dysfunction. It is a sport-style brace connected to a custom corrected foot orthodic that fits into most lace-up footwear (including athletic shoes). It is also light weight and more cosmetically appealing than traditionally prescribed ankle foot orthosis. The Arizona Brace, California Brace or Gauntlet Brace may also be recommended depending on your needs. 
Surgical Treatment
The indications for surgery are persistent pain and/or significant deformity. Sometimes the foot just feels weak and the assessment of deformity is best done by a foot and ankle specialist. If surgery is appropriate, a combination of soft tissue and bony procedures may be considered to correct alignment and support the medial arch, taking strain off failing ligaments. Depending upon the tissues involved and extent of deformity, the foot and ankle specialist will determine the necessary combination of procedures. Surgical procedures may include a medial slide calcaneal osteotomy to correct position of the heel, a lateral column lengthening to correct position in the midfoot and a medial cuneiform osteotomy or first metatarsal-tarsal fusion to correct elevation of the medial forefoot. The posterior tibial tendon may be reconstructed with a tendon transfer. In severe cases (stage III), the reconstruction may include fusion of the hind foot,, resulting in stiffness of the hind foot but the desired pain relief. In the most severe stage (stage IV), the deltoid ligament on the inside of the ankle fails, resulting in the deformity in the ankle. This deformity over time can result in arthritis in the ankle.
Adult Aquired FlatFeet Causes And Treatments
Another common term for this condition is Posterior Tibial Tendon Dysfunction (PTTD). There is a cause-effect relationship between pronation, flatfoot deformity and subsequent tenosynovitis of the posterior tibial tendon. Mechanical irritation of the tendon may lead to synovitis, partial tearing and eventually full rupture of the tendon. Other structures, including ligaments and the plantar fascia, have also been shown to contribute to the arch collapsing. As the deformity progresses, these structures have been shown to attenuate and rupture as well. In later stages, subluxation of various joints lead to a valgus rearfoot and transverse plane deformity of the forefoot. These deformities can become fixed and irreducible as significant osteoarthritis sets in.

Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot. Sometimes this can be a result of specific trauma, but usually the tendon becomes injured from wear and tear over time. This is more prevalent in individuals with an inherited flat foot but excessive weight, age, and level of activity are also contributing factors.
Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
In diagnosing flatfoot, the foot & Ankle surgeon examines the foot and observes how it looks when you stand and sit. Weight bearing x-rays are used to determine the severity of the disorder. Advanced imaging, such as magnetic resonance imaging (MRI) and computed tomography (CAT or CT) scans may be used to assess different ligaments, tendons and joint/cartilage damage. The foot & Ankle Institute has three extremity MRI?s on site at our Des Plaines, Highland Park, and Lincoln Park locations. These extremity MRI?s only take about 30 minutes for the study and only requires the patient put their foot into a painless machine avoiding the uncomfortable Claustrophobia that some MRI devices create.
Non surgical Treatment
Initial treatment for most patients consists of rest and anti-inflammatory medications. This will help reduce the swelling and pain associated with the condition. The long term treatment for the problem usually involves custom made orthotics and supportive shoe gear to prevent further breakdown of the foot. ESWT(extracorporeal shock wave therapy) is a novel treatment which uses sound wave technology to stimulate blood flow to the tendon to accelerate the healing process. This can help lead to a more rapid return to normal activities for most patients. If treatment is initiated early in the process, most patients can experience a return to normal activities without the need for surgery.

Surgical Treatment
For those patients with PTTD that have severe deformity or have not improved with conservative treatments, surgery may be necessary to return them to daily activity. Surgery for PTTD may include repair of the diseased tendon and possible tendon transfer to a nearby healthy tendon, surgery on the surrounding bones or joints to prevent biomechanical abnormalities that may be a contributing factor or both.